Evaluation of Suspicious Spots

Biopsy and Examination Under the Microscope
When a spot is suspicious, the health care provider will often perform a skin biopsy to determine if the spot is cancerous. In this surgical procedure, a piece (or all) of the spot is cut out and is processed. A specialist will look at the processed material under the microscope to see if it looks like melanoma. While pathologic examination of a biopsy sample is considered the gold standard for the diagnosis of melanoma, this method has limitations:
- A biopsy is a procedure that is needed to make a diagnosis of melanoma. But because choosing which lesion to biopsy can be challenging, most lesions that are biopsied due to concern that they could be melanoma will turn out to be benign (noncancerous). This means that a lot of the spots are probably not biopsy worthy. But some providers follow the old adage, “If in doubt, cut it out.”
- Biopsies increase the risk of bleeding, scarring, and infection
- Not all areas can be easily biopsied because of the way the skin lies or because of risk of bleeding (eg, the scalp, side of the nose, or the shin)
- Some people may want to avoid biopsies. If you have diabetes or a bleeding disorder, you may be concerned with complications. Also, some people have anxiety about the cutting procedure
- Sometimes, a review of the biopsy can miss some melanomas or diagnose some noncancerous spots as melanomas. Why does this happen? First, a biopsy and pathologic examination often looks at only a piece of the spot, so it’s possible that the part of the spot that contains the melanoma is not evaluated. Secondly, not all of the specialists reviewing the specimens agree on what is a melanoma and what is not. That’s one reason why a second opinion can be helpful when you have your pathology read.
Non-Invasive Options
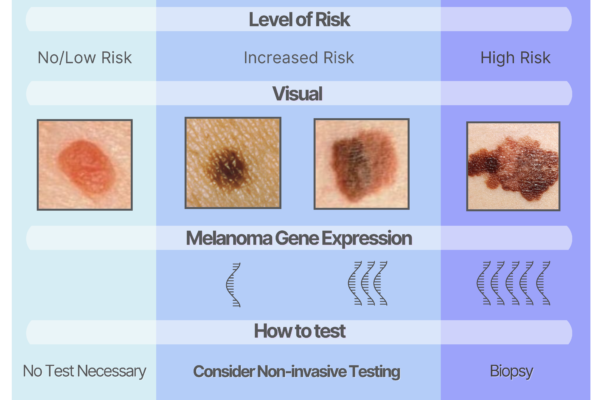
As mentioned, not all spots are biopsy worthy but when there is doubt, some practitioners don’t have any other option but to cut the spot to test it. In reality, most spots fall along a continuum in terms of how suspicious they are (Figure 1). Some moles are so bland and normal looking that an experienced provider can immediately determine that they have no risk for melanoma and therefore are not biopsy worthy. At the other end of the spectrum, some spots are so clearly melanoma (eg, the image at the right that has all the ABCDE features), they will definitely require a biopsy. Not visible to the eye, but detectable with special tools, certain melanoma genes are expressed more frequently as spots progress and serve as markers of increased melanoma risk. The challenging cases are the ones in the middle zone—they seem to be potentially suspicious to the eye, but it’s not clear how high the risk is for melanoma. So, providers often biopsy these out of an abundance of caution. However, if the provider has the right non-invasive tools, they can often get a better assessment of these middle-ground cases without cutting.
Figure 1. Spectrum of risk for melanoma based on visualization and genetic testing of spots. The diagram also addresses the use of non-invasive testing for spots that are suspicious but not clearly melanoma upon visual examination.
As mentioned in the above Figure, your provider may be able to use a range of non-invasive tools to evaluate your spot(s). The Table illustrates some of the non-invasive tools your provider may use to evaluate your suspicious spots.
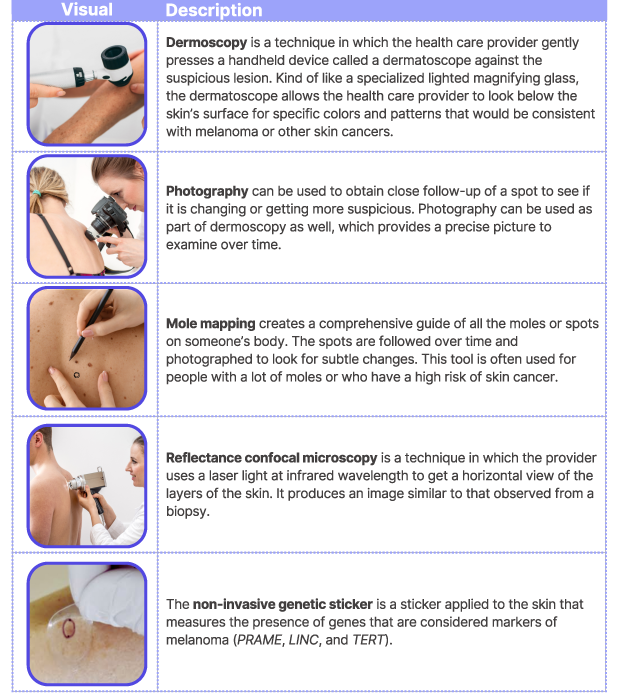
These tools can help your provider decide which of your spots are high risk enough that they warrant a biopsy. It’s helpful to ask your provider if they have these tools and whether they can be used for any of your spots.
